Home > Conditions Treated > Cartilage Damage


Osteochondritis Dissecans a form of cartilage damage involving cracks, divots, or wear of the cartilage on the surface of a joint. This damage may be related to chronic wear and tear from misaligned joint surfaces or attributed to trauma or injury including repetitive joint stress. This results in microfractures which interrupt the blood supply to the underlying bone causing changes in joint architecture. (Other causes include ischemia, hereditary factors, rapid growth and calcium/phosphorus deficiencies or imbalances.)

The lack of direct blood supply means cartilage has very limited capacity to heal and repair. Therefore, cartilage defects will generally remain chronic and unhealed resulting in longstanding pain. The joint cartilage may fragment further over time causing loose bodies of cartilage or bone within the joint and grinding with movement of the joint.
Cartilage or osteochondral defects can occur in any joint but are frequently involve the ankle joint. Sudden ankle inversion sprains (i.e. sole of foot twisting toward the body) are the usual culprit. Most of the pain is usually associated with the sprain but when joint pain lingers long after the sprain has healed, an osteochondral defect should be suspected. In osteochondritis dissecans, pain and inflammation are often seen. Patients with these lesions usually complain of pain with activity.
Often mechanical symptoms such as catching, locking or buckling. A limitation in range of motion is common due to inflammation or bone/cartilage fragments. Grinding within the joint (crepitus) is also common.
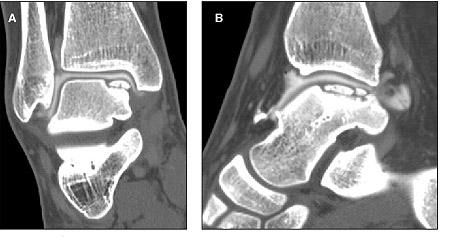
The diagnosis of osteochondritis dissecans is usually made on the basis of imaging. X-ray, CT, MRI or ultrasound can be used to see defects in cartilage surfaces, damage to subchondral (i.e. under cartilage) bone and the presence of loose bodies.
Traditionally, the treatment of Osteochondral defects has involved surgery with prolonged recovery times. Microfracture repair with open or arthroscopic approach has involved drilling of cartilage defects into the subchondral bone. This allowed bleeding from the subchondral bone into the joint. The blood would facilitate the formation of scar thus healing the injury.
Now, Regenerative Medicine procedures are replacing surgery as an effective treatment. The aim of using regenerative medicine is to support your body’s self-healing processes, reverse disease progression and suppress inflammatory reactions that can worsen pain, leading to symptom relief and recovery of function.
We utilize regenerative medicine procedures including patients’ own Cells to repair the joint naturally. Regenerative Cells exist in high concentrations in bone marrow which can be aspirated with minimal discomfort, and then injected into the affected area often with concentrated Platelet Rich Plasma. Platelet Rich Plasma has a high concentration of growth factors that can change the environment in the joint from inflammatory to healing and regenerating.
Although Orthobiologic Cell Therapy is considered by some people to be experimental, various research studies show that some marrow aspirate concentrate and platelet rich plasma injections may provide excellent relief from joint and musculoskeletal pain and ongoing inflammation.
600 Worcester Rd, Ste 301,
Framingham, MA 01702
This information is for educational purposes only and is NOT intended to replace the care or advice given by your physician. Always seek the advice of your physician or other qualified health provider before starting any new treatment or with any questions you may have regarding a medical condition. For more information see our Medical Disclaimer.